Helpful Articles
From Our Team

SORT BY TOPIC

Public Health,
Healthcare Technology
Top Public Health Trends for 2026
READ MORE >

Practice Management
How to Improve Mental Health in the Workplace for Healthcare
READ MORE >

Patagonia Health News
LHDs Leverage EHR to Strengthen SDOH Screening and Referrals
READ MORE >

Healthcare Technology
Choosing an EHR with Exceptional Support & Service for Health Care Teams
READ MORE >

Public Health,
Interoperability
The $50 Billion RHT Program: Why Local Health Departments Drive Rural Transformation
READ MORE >

Public Health
Public Health Emergency Preparedness Guide
READ MORE >

Public Health,
Patient Experience
Community Engagement and Health Improvement Strategies
READ MORE >

Public Health,
Financial Wellness
Turning Public Health Data into Action: A Leader's Guide
READ MORE >

Public Health,
Financial Wellness
How Rural Health Departments Can Thrive with EHRs
READ MORE >

Healthcare Technology
The Complete History of Electronic Health Records
READ MORE >

Medical Billing,
Healthcare Technology
Why Every School Needs an EHR System
READ MORE >

Patagonia Health News
Patagonia Health Named 2025 Triangle Fast 50 Winner
READ MORE >

Public Health,
Healthcare Technology
Enhancing Patient Care with EHRs for Public Health Nurses
READ MORE >

Behavioral Health,
Public Health
HIPAA-Compliant Notes: Protect Patient Data in Clinical Documentation
READ MORE >

Behavioral Health,
Practice Management
Psychology vs. Psychiatry
READ MORE >

Behavioral Health,
Interoperability
School Mental Health Assessments for Early Intervention
READ MORE >

Public Health
Community Health vs. Public Health
READ MORE >

Public Health,
Healthcare Technology
How EHRs Strengthen Public Health's Fight Against Opioid Addiction
READ MORE >

Patagonia Health News
Patagonia Health Named One of Triangle's Best Places to Work
READ MORE >

Patient Experience
Understanding the Social Determinants of Health
READ MORE >

Public Health,
Healthcare Technology
How EHRs Support Public Health Programs and Improve Outcomes
READ MORE >

Behavioral Health,
Healthcare Technology
7 Reasons to Get a Cloud-Based EHR for Mental Health
READ MORE >

Behavioral Health,
Public Health
9 Must-Have EHR Features for Small Practices
READ MORE >

Behavioral Health,
Healthcare Technology
How EHRs Revolutionize Mental Health Care for Anxiety and Depression
READ MORE >

Behavioral Health,
Healthcare Technology
Best EHR for Private Practice: A Comprehensive Guide for Therapists
READ MORE >
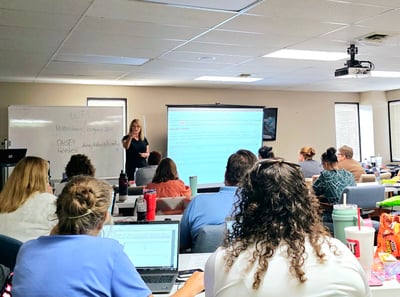
Patagonia Health News
Patagonia Health Celebrates the Success of User Group Events
READ MORE >

Practice Management,
Healthcare Technology
Best Features for a Practice Management Software
READ MORE >

Behavioral Health,
Healthcare Technology
What to Look for in Substance Abuse Software for Your Treatment Center
READ MORE >

Data Security,
Expert Interviews
Expert Interview: Aligning Healthcare System Updates with Regulations
READ MORE >

Behavioral Health,
Data Security
Choosing a HIPAA-Compliant Mental Health EHR
READ MORE >

Behavioral Health,
Healthcare Technology
How EHR Systems Streamline Mental Health Assessments
READ MORE >

Behavioral Health,
Medical Billing
Finding the Right Billing Software for Therapists
READ MORE >

Behavioral Health,
Healthcare Technology
How EHRs Empower Trauma-Informed Care
READ MORE >

Public Health,
Patient Experience
How an EHR Improves Patient Safety
READ MORE >

Behavioral Health,
Medical Billing
How Accounting and Billing Technology Empowers Therapists
READ MORE >

Behavioral Health,
Interoperability
How to improve Interoperability in Healthcare
READ MORE >

Behavioral Health
Mastering Clinical Documentation: A Practical Guide to Progress Notes
READ MORE >

Behavioral Health
The Best EHR for Psychiatrists
READ MORE >

Patagonia Health News
Patagonia Health Wins 2025 Stevie Award
READ MORE >

Behavioral Health,
Healthcare Technology
The Ultimate Guide to EHR Implementation for Mental Health Clinics
READ MORE >

Data Security,
Expert Interviews
Expert Interview: Harbi Dhanjal | Securing Your Health Organization
READ MORE >

Patagonia Health News
Patagonia Health Wins Triangle Business Fast 50 Award 2024
READ MORE >

Financial Wellness
Is the Sun Setting on Your Current EHR System?
READ MORE >

Patagonia Health News
Enhanced Custom Forms App by Patagonia Health
READ MORE >
Patagonia Health News
Introducing Patagonia Health Academy (eLearning Module)
READ MORE >

Behavioral Health
Breaking the Cycle: Deflection and Diversion Prevent Opioid Overdose
READ MORE >
Behavioral Health,
Practice Management
Weaving the Golden Thread for Clinical Documentation
READ MORE >

Healthcare Technology,
Expert Interviews
Expert Interview: Jolie Rollins & Monique Dever
READ MORE >

Industry News,
Interoperability
How the HTI Rules Are Reshaping Health Data
READ MORE >

Behavioral Health,
Industry News
ASAM 4th Edition Criteria for Behavioral Health Clinicians
READ MORE >

Behavioral Health
Tools for Mobile Integrated Health Services in Behavioral Health
READ MORE >

Behavioral Health
Benefits of Mobile Integrated Health for Behavioral Health
READ MORE >

Patagonia Health News
Patagonia Health Wins Gold Award for Sales and Customer Service
READ MORE >

Patagonia Health News
Patagonia Health Launches Ideas Portal for Feature Requests
READ MORE >

Medical Billing,
Public Health
They’re Going Around: Local Health Department Billing Headaches
READ MORE >

Medical Billing,
Financial Wellness
Improve Your Collections Process with 5 Easy Changes
READ MORE >

Patagonia Health News
Patagonia Health Promotes Prasad Naik as VP of Finance
READ MORE >

Patagonia Health News
Patagonia Health Celebrates 15 Years of Service
READ MORE >

Patagonia Health News
Patagonia Health Streamlines its Clinical Form Update Process
READ MORE >

Patagonia Health News
Patagonia Health Offers FPAR 2.0 Reporting
READ MORE >

Financial Wellness
Sustainable Healthcare: The Benefits of Going Paperless
READ MORE >

Interoperability,
Financial Wellness
Why Should I Choose a Cures Act Certified EHR?
READ MORE >

Patient Experience
6 Strategies to Boost Patient Engagement
READ MORE >

Interoperability,
Financial Wellness
School Health: Why Should My EHR Be FERPA Certified?
READ MORE >

Patient Experience,
Healthcare Technology
How Your EHR Can Improve Health Equity
READ MORE >

Financial Wellness
Managing Your EHR Implementation Timeline
READ MORE >

Public Health
The 5 A’s for Smoking Cessation Interventions
READ MORE >

Financial Wellness,
Healthcare Technology
EHRs Can Improve Efficiency of High Volume Immunizations
READ MORE >

Patagonia Health News
Introducing our New Appointment Adherence App
READ MORE >

Patagonia Health News
“Patagonia Health Pioneers” Recognized for 10+ Years of Service
READ MORE >

Patagonia Health News
Patagonia Health Certified as an NC Minority-Owned Business
READ MORE >

Patagonia Health News
Patagonia Health Wins 2023 Stevie Award
READ MORE >

Public Health,
Healthcare Technology
How EHRs Help Public Health Win the War Against TB
READ MORE >

Financial Wellness
10 Questions to Ask in Your EHR RFP
READ MORE >

Interoperability,
Expert Interviews
Expert Interview: Komal Sadani
READ MORE >

Industry News,
Financial Wellness
The Mental Health Matters Act– EHR Functionalities for School Health
READ MORE >
Patagonia Health News
Patagonia Health Joins Forces with Fairfax County Health Department
READ MORE >

Patagonia Health News
Patagonia Health Wins Triangle Business Fast 50 Award
READ MORE >

Financial Wellness
EHR Selection and Implementation Success: Common Q & As
READ MORE >

Patient Experience,
Patient Portal
How an EHR Improves Patient Care
READ MORE >

Healthcare Technology,
Expert Interviews
Expert Interview: Don Sargent
READ MORE >

Financial Wellness
Your Modern-day EHR Can't Be DIY
READ MORE >

Behavioral Health,
Public Health
Fentanyl Crisis - How an EHR Can Help
READ MORE >

Patient Experience,
Telehealth
Providing a Better Telehealth Experience
READ MORE >

Behavioral Health,
Public Health
Community Violence: How an EHR can Help
READ MORE >

Financial Wellness,
Healthcare Technology
How EHRs Reduce Medical Costs for Providers
READ MORE >

Public Health,
Healthcare Technology
How an EHR Can Support Men’s Health
READ MORE >

Behavioral Health,
Telehealth
Telehealth Group Therapy Functionality Now Expanded
READ MORE >

Patagonia Health News
Patagonia Health Connects to Multiple State-Run Immunization Registries
READ MORE >

Telehealth,
Financial Wellness
Inflation and the Need for Telehealth Access
READ MORE >

Financial Wellness
EHR Total Cost of Ownership: Pricing You can Trust
READ MORE >

Patagonia Health News
Patagonia Health Wins 2022 Stevie Award!
READ MORE >

Patagonia Health News
Patagonia Health Offers Free 2-Factor Authentication for EHR
READ MORE >

Healthcare Technology
Understanding the Differences: EMR vs EHR
READ MORE >

Interoperability,
Healthcare Technology
Public Health 3.0 Framework and EHRs to Support it
READ MORE >

Healthcare Technology
EHR Apps Study Spells the Future of Healthcare
READ MORE >

Public Health
Opioid Abuse Prevention in Chronic Pain Patients
READ MORE >

Behavioral Health
Behavioral Health Trends for 2026
READ MORE >

Behavioral Health,
Public Health
Adolescent Mental Health Support for Caregivers and Health IT Leaders
READ MORE >

Financial Wellness
Tips to Support Employee Mental Health
READ MORE >

Financial Wellness
Employee Retention Strategies in Healthcare
READ MORE >

Industry News
Major Healthcare Regulations for 2026
READ MORE >

Financial Wellness
Personalization, Configuration and Customization in EHR Design
READ MORE >

Financial Wellness
How to Migrate data to a new EHR Successfully
READ MORE >

Financial Wellness
How to Train New Employees in your EHR when you‘re Busy
READ MORE >

Public Health
How EHRs support Diabetes & Smoking Cessation Programs
READ MORE >

Practice Management,
Healthcare Technology
Everything Public Health Professionals Need to Know About FPAR 2.0 Reporting
READ MORE >

Financial Wellness
Implementation Best Practices for EHRs
READ MORE >

Financial Wellness
Cloud Based Complete EHR Systems: Solving the Build it or Buy it Debate
READ MORE >

Patagonia Health News
Jonathan Strange Hired as Patagonia Health's Clinical Director
READ MORE >
.jpeg?width=400&name=AdobeStock_1085889895%20(1).jpeg)
Financial Wellness
How to Know When to Transition to Another EHR
READ MORE >

Behavioral Health
Adolescent Behavioral Health: Solutions for a National Emergency
READ MORE >

Behavioral Health,
Public Health
Behavioral Health Integration: EHR Support for Co-Treatment
READ MORE >

Patient Experience
Social Determinants of Health: Two Perspectives
READ MORE >

Interoperability,
Practice Management
EHR Interoperability: Playing Well with Others
READ MORE >

Telehealth
Telehealth or Virtual Meetings? How to tell the difference
READ MORE >

Patient Experience,
Healthcare Technology
Whole Person Care and the Role of EHRs
READ MORE >

Patient Experience,
Practice Management
Texting is Now a Vital Part of Patient Communications
READ MORE >

Behavioral Health
IM+Cans: A Paradigm Shift in Behavioral Health Clinical Tools
READ MORE >

Interoperability,
Practice Management
The Cures Act: How EHRs Play a Part
READ MORE >

Industry News,
Interoperability
Trend of Health Information Exchanges Merging and Linking
READ MORE >

Patagonia Health News
Patagonia Health Launches Time and Effort Tracking App
READ MORE >

Data Security
How to Defend Against the Rise of Ransomware
READ MORE >

Financial Wellness
Finding a Trustworthy EHR Vendor
READ MORE >

Patagonia Health News
Patagonia Health Joins the Carequality Network
READ MORE >
Behavioral Health,
Telehealth
Guidelines for Using Telehealth for Group Therapy
READ MORE >

Financial Wellness,
Patient Portal
Alleviate Staffing Shortages with an EHR and Patient Self Services
READ MORE >

Patagonia Health News
Patagonia Health Hires Clark McKenna: Strategic Account Executive
READ MORE >

Financial Wellness
EHR Implementation Success: 7 Tips
READ MORE >

Data Security
Staff Moves: Increasing Security and Protecting Patient Data
READ MORE >

Patagonia Health News
Customer Service Success: Patagonia Health Wins 2021 Stevie Award
READ MORE >

Telehealth
Benefits of an Embedded EHR Telehealth Tool
READ MORE >

Patagonia Health News
Patagonia Health now supporting MS Edge Browser
READ MORE >

Financial Wellness,
Healthcare Technology
Use a Cloud-Based EHR to Reduce Costs
READ MORE >

Financial Wellness
How to Evaluate EHR Solutions
READ MORE >

Public Health
Modernize Public Health Infrastructure to Defend Against Emerging Viruses
READ MORE >

Patagonia Health News
Patagonia Health Piloting New Contactless Patient Experience App
READ MORE >

Healthcare Technology
Usability versus Learnability in EHR User Interface
READ MORE >

Financial Wellness
Shopping for an EHR - 8 things to find out First
READ MORE >

Industry News
Do Individuals have to Disclose Vaccination Status?
READ MORE >

Behavioral Health
EHR Implementation for Behavioral Health Challenges
READ MORE >

Data Security
Protect Patient Data from CyberAttack: 5 EHR Security Features
READ MORE >

Financial Wellness
Combat Digital Burnout with these 3 EHR Solutions
READ MORE >

Healthcare Technology
EHRs for E-Prescriptions and Drug Monitoring Programs
READ MORE >
Medical Billing,
Financial Wellness
Bill to Adopt the CCBHC Medicaid Demonstration Nationwide
READ MORE >

Financial Wellness
Optimize IT Spending: How EHR Support Affects your Bottom Line
READ MORE >

Financial Wellness
Traumatic Stress: Protecting Health Staff
READ MORE >

Industry News,
Data Security
Internet Explorer Security is going away: Is it taking yours with it?
READ MORE >

Public Health
Communication Tips for the Importance of Immunizations
READ MORE >

Patagonia Health News
Patagonia Health Offers Interface to PHIN Public Health Information Network
READ MORE >

Public Health,
Industry News
The Threat to Mental Health during COVID-19 & How Practitioners Can Help
READ MORE >

Patagonia Health News
Patagonia Health: Adapt & Innovate, At Speed
READ MORE >

Patagonia Health News
Patagonia Health Supports Mass Vaccination Campaigns
READ MORE >

Behavioral Health
The Golden Thread: Tell a Story of the Entire Treatment Journey
READ MORE >

Patagonia Health News
Patagonia Health EHR Wins Bronze Stevie Award for Customer Service
READ MORE >
Patagonia Health News
Patagonia Health Develops Integrated Telehealth Solution
READ MORE >
.jpeg?width=400&name=AdobeStock_532389552%20(1).jpeg)
Telehealth
Telehealth is Here to Stay
READ MORE >

Behavioral Health,
Public Health
Telehealth Best Practices: Enhancing Webside Manner
READ MORE >

Behavioral Health
Mental Health Awareness Month
READ MORE >

Public Health,
Practice Management
Contact Tracing and Next Steps
READ MORE >
Patagonia Health News
Patagonia Health Connected with Carequality Interoperability Framework
READ MORE >
Public Health,
Patagonia Health News
Patagonia Health Featured in KLAS COVID-19 Technology Guide
READ MORE >

Telehealth,
Industry News
New Rules for Telehealth Technology
READ MORE >
Patagonia Health News
Patagonia Health Launches COVID-19 Risk Assessment Tool
READ MORE >

Financial Wellness
Becoming a Certified Community Behavioral Health Clinic (CCBHC): Part 2
READ MORE >

Behavioral Health
Becoming a Certified Community Behavioral Health Clinic (CCBHC): Part 1
READ MORE >

Behavioral Health,
Interoperability
Why Health Information Exchange is Important for EHR Use
READ MORE >

Interoperability
What is HL7?
READ MORE >

Behavioral Health
Inside Behavioral Health: What is a CCBHC?
READ MORE >

Behavioral Health,
Public Health
How Interoperability Strengthens Whole-Person Care
READ MORE >

Industry News
North Carolina Requires Opioid E-Prescribe
READ MORE >

Medical Billing,
Financial Wellness
Connecting to NC HealthConnex
READ MORE >

Financial Wellness,
Healthcare Technology
Ten Indicators That You Should Replace and Modernize Your EHR System
READ MORE >

Interoperability
What is the NC HIE?
READ MORE >

Financial Wellness
Will Your Staff Adopt Your New EHR Software?
READ MORE >

Patagonia Health News
Patagonia Health Welcomes Harbi Dhanjal as VP of Engineering
READ MORE >

Patagonia Health News,
Customer Story
Mental Health Association in Passaic County Partners with Patagonia Health
READ MORE >

Patagonia Health News
Patagonia Health Wins 2019 Customer Service Award
READ MORE >

Financial Wellness
6 Ways to Optimize Your EHR
READ MORE >

Behavioral Health,
Interoperability
CMS and ONC Propose New Rules for Interoperability
READ MORE >

Patagonia Health News
Site Code Filter Added to Billing System
READ MORE >

Digital Voice Assistants in Healthcare
READ MORE >

Financial Wellness,
Healthcare Technology
How to Choose the Right EHR for Your Organization
READ MORE >

Financial Wellness
3 Critical Questions for Choosing Your EHR
READ MORE >
Patagonia Health News
Patagonia Health Expands EHR for Home Visit Intervention Tracking
READ MORE >

Patagonia Health News
Vaccine Inventory App is Enhanced
READ MORE >

Patagonia Health News
Custom Reports Added to EHR
READ MORE >
Patagonia Health News
Patient Consent Forms Are Now Editable
READ MORE >

Patagonia Health News
Patagonia Health Hires Amos Slaymaker as VP of Sales
READ MORE >
Patagonia Health News
Bi-directional Lab Orders Interface
READ MORE >

Patagonia Health News
Behavioral Health Agencies Successfully Connected to NCHIE via Patagonia Health EHR
READ MORE >
Patagonia Health News
Patagonia Health's EHR Software Earns ONC Health IT Certification
READ MORE >

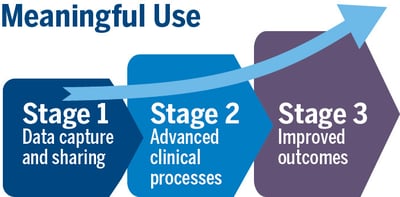
Patagonia Health News
Meaningful Use Stage 3 Certification is Complete!
READ MORE >

Behavioral Health
Having the Right Tool at the Right Time
READ MORE >
Financial Wellness
Not all EHR Vendors are Created Equal
READ MORE >

Behavioral Health,
Public Health
Setting the Stage: Patient Satisfaction Begins at Check-In
READ MORE >

Financial Wellness
EHR Support and Training: What Sets the Best Apart
READ MORE >
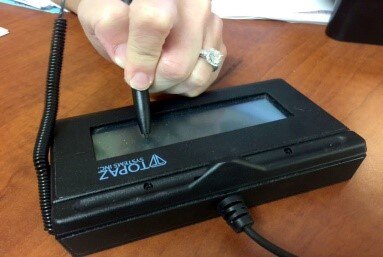
Patagonia Health News
Patagonia Health to Roll out New Patient ID Scanner
READ MORE >

Public Health
E-cigarette Effects and Hazards
READ MORE >
Patagonia Health News
Patagonia Health Makes Top 10 Most Trusted EHR Vendors List
READ MORE >

Behavioral Health
EHR Use Case for Smoking Behavior Cessation
READ MORE >

Patagonia Health News
Patagonia Health Wins GOLD!
READ MORE >

Public Health
When battling the Flu season, EHR technology can help
READ MORE >

Financial Wellness
Switching from Legacy to Cloud Based EHR
READ MORE >

Patagonia Health News
Patagonia Health EHR Wins 2018 GOLD Stevie® for Customer Service
READ MORE >
Patagonia Health News
Patagonia Health adds New eCQMs to EHR
READ MORE >

Financial Wellness
Will Mental Health Providers get EHR incentives
READ MORE >

Healthcare Technology
3 Ways (+1 bonus) EHR Data Helps Calm the Opioid Crisis
READ MORE >
Financial Wellness
In the Aftermath of Hurricanes, Your Choice of EHR Matters
READ MORE >

Patagonia Health News
Patagonia Health Named Top 10 EHR Solution by Healthcare Tech Magazine
READ MORE >

Financial Wellness
Is Your EHR Vendor Legit? The Top 4 things to Find Out
READ MORE >

Public Health,
Interoperability
Immunization Registries: Benefits for Healthcare Organizations
READ MORE >

Data Security
2-Factor Authentication: A shield for PHI against hackers
READ MORE >
Patagonia Health News
Save Paper and Time with built-in Electronic Patient Consent Forms
READ MORE >

Behavioral Health
Pushing Mental Healthcare Quality to the Forefront
READ MORE >

Patagonia Health News
Patagonia Health Supports 2-Factor Authentication
READ MORE >
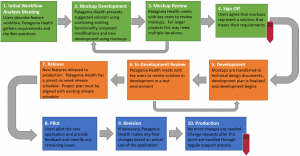
Public Health
User-Centered Design Process
READ MORE >
Public Health,
Healthcare Technology
Vaccine-Preventable Diseases: Public Health vs Personal Choice
READ MORE >

Public Health,
Patient Experience
Keeping Patient Safety a Priority in your Health Center
READ MORE >
Behavioral Health,
Public Health
Health in All Policies – What it means for Mental Health
READ MORE >

Financial Wellness
The 6 Steps EHR Selection & Implementation: Plan for Planning
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Julia Caplan, MPP, MPH
READ MORE >

Patagonia Health News
Patagonia Health Wins Bronze Stevie Award for Customer Service Excellence
READ MORE >

Data Security
4 Reasons Not Conducting a Security Risk Assessment Can Cost You Money
READ MORE >

Patagonia Health News
Patagonia Health Partners Offers Security Risk Assessment
READ MORE >

Public Health
A Balancing Act for Public Health Departments. 3 things to focus on
READ MORE >
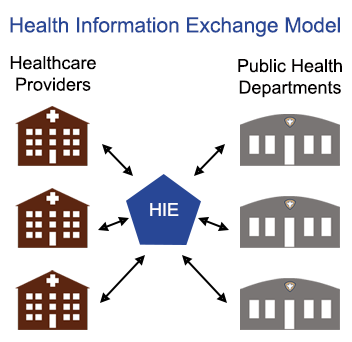
Public Health,
Interoperability
Is the value of participating in Health Information Exchange (HIE) worth it for public health departments?
READ MORE >
Industry News
Dealing with Change: Managing the Uncertainty in Healthcare
READ MORE >

Data Security
8 Common HIPAA Breaches to Avoid and What to Look for in Your EHR
READ MORE >

Practice Management
Check your Tables: Common UDS Reporting Mistakes
READ MORE >

Financial Wellness
Three Steps to Make the Most of EHR Vendor Demos
READ MORE >

Patient Experience,
Expert Interviews
Expert Interview: Marni Mason, BSN, MBA
READ MORE >
Behavioral Health,
Industry News
Addiction in America: A $420 Billion-dollar fight in Behavioral Health
READ MORE >
Medical Billing,
Financial Wellness
Quality patient care with new Medicare Payment System (MACRA)
READ MORE >

Industry News
Affordable Care Act Open Enrollment and Community Health (FQHC)
READ MORE >
Patagonia Health News
Patagonia Health Ranks 865 on Inc. 5000 Fastest-Growing Companies List
READ MORE >

Patagonia Health News
Boost Productivity and Cut Costs with Electronic Fax
READ MORE >

Behavioral Health,
Public Health
Without a certified EHR, clinics are missing out on benefits of eRX
READ MORE >

Medical Billing,
Financial Wellness
How Accountable Care Organizations Improve Community Health
READ MORE >
Financial Wellness
Five Steps to a Successful EHR Data Migration
READ MORE >

Patagonia Health News
Streamline your community health center with improved UDS Reporting options
READ MORE >

Financial Wellness
7 Levels of Service & Support You Should Demand from Your EHR Vendor
READ MORE >

Patagonia Health News
Quick Photo Capture Currently Now in Pilot Mode
READ MORE >

Patagonia Health News
New Bar Code Scanner Option for Immunization App
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Matthew Simon, MA, GISP
READ MORE >

Patagonia Health News
Patagonia Health Expands; Relocates Headquarters
READ MORE >

Behavioral Health,
Public Health
EHR Incentive Program Unites Behavioral and Public Health Agencies
READ MORE >

Industry News,
Financial Wellness
FQHC Guide to the 340B Drug Program
READ MORE >

Medical Billing,
Financial Wellness
Are You Down with PPS?
READ MORE >

Financial Wellness
21 Steps to a Successful EHR Implementation
READ MORE >
Practice Management,
Data Security
Understand HIPAA violations to prevent them from happening to you
READ MORE >

Public Health
What's in your Family Planning Annual Report? (FPAR)
READ MORE >

Financial Wellness,
Healthcare Technology
Time is Money: FQHC Requirements from their EHR
READ MORE >

Patagonia Health News
Workflow Analysis & Optimization Services
READ MORE >

Patagonia Health News
Patagonia Health Wins 2016 Bronze Stevie® Award
READ MORE >

Interoperability,
Expert Interviews
Expert Interview: Ross D. Martin, MD, MHA
READ MORE >

Patagonia Health News
Patagonia Health makes the list of most promising RTP tech companies
READ MORE >

Medical Billing,
Expert Interviews
Expert Interview: Laurie A. Poulin, CPC
READ MORE >
Financial Wellness
Will Your EHR Vendor Conduct Workflow Analysis for Public Health?
READ MORE >
Patagonia Health News
Patagonia Health Carries Customers Safely Across the ICD-10 Threshold
READ MORE >
Public Health
Public Health Departments: Improve Workflow AND EHR Implementation
READ MORE >

Public Health
Credentialing Made Easier for Local Health Departments
READ MORE >

Financial Wellness
EHR User Groups: The Benefits of Group Learning
READ MORE >

Patient Experience,
Patient Portal
The benefits of an EHR from the patient’s perspective
READ MORE >

Industry News,
Practice Management
Implementing EHRs at Title X Agencies
READ MORE >

Patagonia Health News,
Customer Story
Cleveland County Health Dept: Public Health EHR Implementation
READ MORE >

Patagonia Health News
Patagonia Health Ranks Top 5% on Inc. 5000 List
READ MORE >

Public Health,
Industry News
Patagonia Health EHR; Making things easier for healthcare professionals
READ MORE >
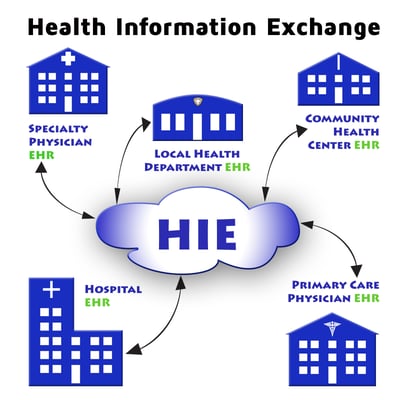
Interoperability
What is Health Information Exchange and Why is it Important for EHR use?
READ MORE >
Practice Management
What is your Strategy for Medical Record Scanning
READ MORE >
Patagonia Health News,
Customer Story
Rowan County Replaces Legacy EHR Software with Patagonia Health
READ MORE >
Public Health
Working Together: Top 10 Public Health Achievements in 10 year span
READ MORE >

Patagonia Health News,
Customer Story
Patagonia Health Aids County Health Departments to Successful Attestations
READ MORE >

Patagonia Health News
Meaningful Use EHR Incentive Assistance Service
READ MORE >
Data Security
6 Things Your EHR Must Do to Secure Patient Information
READ MORE >
Medical Billing,
Financial Wellness
3 steps to increase reimbursements for public health departments
READ MORE >

Patagonia Health News,
Customer Story
Nash County Health Department Adopts Patagonia Health EHR
READ MORE >

Interoperability,
Practice Management
EHR-HIE Integration: Enhancing Syndromic Surveillance for Public Health
READ MORE >
Medical Billing
Understanding Medicare Incident-To Billing for Public Health
READ MORE >

Medical Billing,
Public Health
ICD-10-CM has big benefits for Public Health!
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Dr. Stephanie Bailey
READ MORE >

Public Health,
Patient Experience
EHR Photo IDs: Unique Patient Identification for Health Departments
READ MORE >

Financial Wellness
The 6 must-haves for an easy to use EHR for Local Health Departments.
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Jan O’Neill
READ MORE >
Public Health,
Interoperability
Timely data is difficult to obtain for urban public health departments
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Kevin Sherin MD, MPH, MBA
READ MORE >
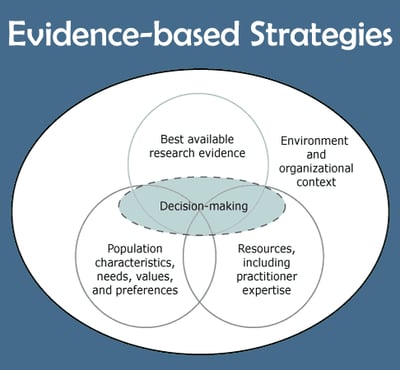
Public Health,
Patient Experience
How can EHR help with Evidence-Based Approach to improving patient health?
READ MORE >
Public Health,
Patient Experience
Are Local Health Departments Ready for Patient Portals?
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Anna Schenck
READ MORE >

Patagonia Health News
EHR Dashboard App for local health departments
READ MORE >

Practice Management,
Expert Interviews
Expert Interview: John Graham, PhD
READ MORE >

Public Health
What is Public Health?
READ MORE >

Industry News,
Practice Management
What’s happening with Title X Family Planning?
READ MORE >
Sure, price is important when buying an EHR.
READ MORE >

Public Health,
Patient Experience
Medical Record Errors: They’re more likely than you think.
READ MORE >

Financial Wellness
7+1 bonus steps for EHR selection for local health departments
READ MORE >

Public Health,
Healthcare Technology
The power of data in a blackout: LHD preparedness & emergency response
READ MORE >
Healthcare Technology
When it comes to EHR adoption, where does public health rank?
READ MORE >

Patient Experience,
Industry News
Why Doctors Resist Mobile Health Despite Patient Demand
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Dr. Susan Zepeda
READ MORE >

Public Health,
Industry News
Are fist-bumps the new handshake for public health?
READ MORE >
Industry News
The Center for Healthy North Carolina releases its latest “Snapshot of Success”
READ MORE >
Public Health,
Patient Experience
How texting is benefiting public health
READ MORE >

Public Health
Pestronk encourages local health department leaders
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Robert Pestronk
READ MORE >
Public Health
Public health and prevention: From behind the scenes to center stage
READ MORE >
Public Health,
Patient Experience
Mobile Apps: Transforming Public Health
READ MORE >

Public Health,
Expert Interviews
Expert Interview: Laura Edwards
READ MORE >
Patagonia Health News
NC HIE Partners with Patagonia Health and NC Office of Rural Health
READ MORE >

Public Health,
Expert Interviews
Expert Interview – Rebecca Williams, MHS, PhD
READ MORE >

Patagonia Health News
Patagonia Health Receives ONC-ACB Certification by Drummond Group
READ MORE >

Patagonia Health News
Public Health Selects Patagonia Health for EHR Billing Solutions
READ MORE >
Patagonia Health News
Patagonia Health Launches Behavioral Health EMR with Built-in Forms
READ MORE >
Patagonia Health News
Patagonia Health EHR is federally certified for Meaningful Use 2011
READ MORE >
Patagonia Health News
Patagonia Health Named Top NC Startup
READ MORE >
Load More
Subscribe for More Helpful Content From the Patagonia Health Team!
Need guidance?
Schedule a free 20-minute consultation.
Have questions about how Patagonia Health can meet your needs? Our team of experts is ready to help.