Helpful Articles
From Our Team

SORT BY TOPIC

Public Health
The 5 A’s for Smoking Cessation Interventions
READ MORE >

Patagonia Health News
Patagonia Health Hires Clark McKenna as New Strategic Account Executive
READ MORE >

Patagonia Health News
Patagonia Health Offers Interface to PHIN Public Health Information Network
READ MORE >

Public Health,
Industry News
The Threat to Mental Health during COVID-19 & How Practitioners Can Help
READ MORE >

Patagonia Health News
Patagonia Health: Adapt & Innovate, At Speed
READ MORE >

Patagonia Health News
Patagonia Health Provides Tools to Public Health Departments for Successful Mass Vaccination Initiatives
READ MORE >

Financial Wellness,
Healthcare Technology
Ten Indicators That You Should Replace and Modernize Your EHR System
READ MORE >

Financial Wellness
Will your staff use and adopt your new Electronic Health Record EHR software?
READ MORE >

Digital Voice Assistants in Healthcare
READ MORE >

Financial Wellness
Best-of-Breed or All-in-One? Which EHR is Right for You?
READ MORE >

Financial Wellness
3 Important - Often Unasked - Questions to Consider when Selecting a new EHR
READ MORE >

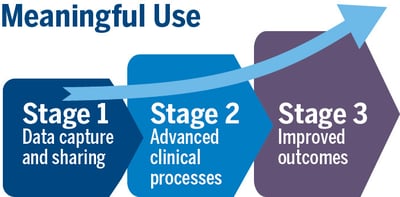
Patagonia Health News
Meaningful Use Stage 3 Certification is Complete!
READ MORE >
Patagonia Health News
Patagonia Health to Roll out New Patient ID Scanner
READ MORE >
Patagonia Health News
Patagonia Health Makes Top 10 Most Trusted EHR Vendors List
READ MORE >
Public Health
When battling Flu season, EHR technology can help!
READ MORE >

Financial Wellness
Switching from Legacy to Cloud Based EHR
READ MORE >

Patagonia Health News
Patagonia Health EHR Wins GOLD Stevie® Award 2018 Customer Service Success
READ MORE >
Patagonia Health News
Patagonia Health adds New eCQMs to EHR
READ MORE >

Financial Wellness
Will Mental Health Providers get EHR Incentives?
READ MORE >

Healthcare Technology
3 Ways (+1 bonus) EHR Data Helps Calm the Opioid Crisis
READ MORE >

Patagonia Health News
Patagonia Health Recognized by Healthcare Tech Outlook Magazine as a Top 10 Most Promising EHR Solution for 2017
READ MORE >

Financial Wellness
Is Your EHR Vendor Legit? The Top 4 things to Find Out
READ MORE >
Patagonia Health News
Save Paper and Time with Patagonia Health’s built-in Electronic Patient Consent Forms
READ MORE >

Patagonia Health News
Patagonia Health Supports 2-Factor Authentication
READ MORE >

Patagonia Health News
Patagonia Health wins Bronze Stevie® Award in the “ Customer Service Success - Technology Industries” for second year
READ MORE >
Public Health,
Interoperability
Is the value of participating in Health Information Exchange (HIE) worth it for public health departments?
READ MORE >

Data Security
8 Common HIPAA Breaches to Avoid and What to Look for in Your EHR
READ MORE >

Financial Wellness
Three Steps to Make the Most of EHR Vendor Demos
READ MORE >
Medical Billing,
Financial Wellness
Clinicians soon to be rewarded for providing quality patient care with new Medicare Payment System (MACRA)
READ MORE >
Patagonia Health News
Inc. Magazine Ranks Patagonia Health #865 on the 35th Annual List of America’s Fastest-Growing Private Companies—the Inc. 5000
READ MORE >

Behavioral Health,
Public Health
Without a certified EHR, clinics are missing out on benefits of eRX
READ MORE >
Financial Wellness
Five Steps to a Successful EHR Data Migration
READ MORE >

Financial Wellness
7 Levels of Service & Support You Should Demand from Your EHR Vendor
READ MORE >

Patagonia Health News
Patagonia Health Expands; Relocates Headquarters
READ MORE >

Behavioral Health,
Public Health
Revised EHR Incentive Program Could Get Behavioral Health and Public Health Agencies on the Same Team
READ MORE >

Financial Wellness
21 Steps to a Successful EHR Implementation
READ MORE >
Practice Management,
Data Security
Understand HIPAA violations to prevent them from happening to you
READ MORE >

Patagonia Health News
Patagonia Health Wins Bronze Stevie® Award in 2016 10th Annual Stevie Awards
READ MORE >

Patagonia Health News
Patagonia Health makes the list of most promising RTP tech companies
READ MORE >
Financial Wellness
Conducting a workflow analysis for public health departments: Will your EHR vendor perform this for you?
READ MORE >
Patagonia Health News
Patagonia Health Carries Customers Safely Across the ICD-10 Threshold
READ MORE >

Public Health
Credentialing Made Easier for Local Health Departments
READ MORE >
Financial Wellness
EHR User Groups: The Benefits of Group Learning
READ MORE >

Patient Experience,
Patient Portal
The benefits of an EHR from the patient’s perspective
READ MORE >

Industry News,
Practice Management
Implementing EHRs at Title X Agencies
READ MORE >

Patagonia Health News,
Customer Story
Cleveland County Health Department Shares Proven Best Practices for a Successful Public Health EHR Implementation
READ MORE >

Patagonia Health News
Patagonia Health Ranks Top 5% on the Inc. 5000 List Fastest Growing Companies
READ MORE >

Public Health,
Industry News
Patagonia Health EHR; Making things easier for healthcare professionals
READ MORE >
Patagonia Health News,
Customer Story
Rowan County Health Department Replaces Legacy EHR Software with Patagonia Health
READ MORE >
Public Health
Working Together: Top 10 Public Health Achievements in 10 year span
READ MORE >

Patagonia Health News,
Customer Story
Patagonia Health Aids County Health Departments to Successful Attestations
READ MORE >
Data Security
6 Things Your EHR Must Do to Secure Patient Information
READ MORE >
Medical Billing,
Financial Wellness
Three easy steps to increase reimbursements for public health departments
READ MORE >

Patagonia Health News,
Customer Story
Nash County Health Department Switches to Patagonia Health EHR to Improve workflow and Meet Meaningful Use Requirements
READ MORE >

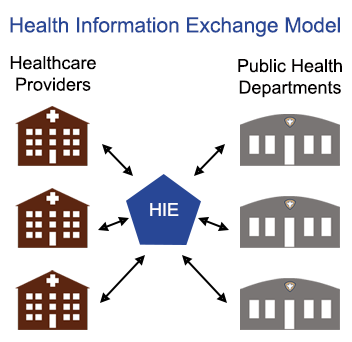
Interoperability,
Practice Management
Connecting to Health Information Exchange (HIE) via EHR - how it helps syndromic surveillance for public health
READ MORE >
Medical Billing
Understanding Medicare Incident-To Billing for Public Health
READ MORE >

Medical Billing,
Public Health
ICD-10-CM has big benefits for Public Health!
READ MORE >

Public Health,
Patient Experience
How can EHR photo IDs help local health departments uniquely identify patients?
READ MORE >
Public Health,
Interoperability
Timely data is difficult to obtain for urban public health departments
READ MORE >
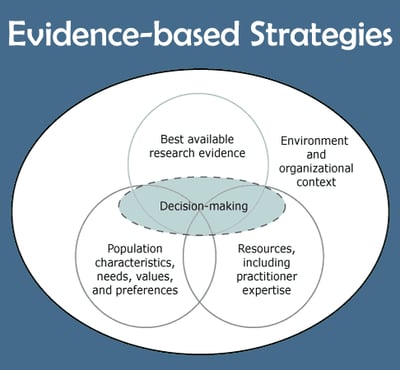
Public Health,
Patient Experience
How can EHR help with Evidence-Based Approach to improving patient health?
READ MORE >
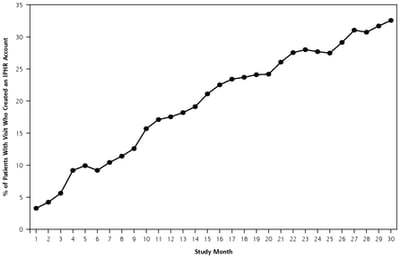
Public Health,
Patient Experience
Are local health departments ready to share medical information via patient portal?
READ MORE >

Patagonia Health News
EHR Dashboard App for local health departments
READ MORE >

Public Health
What is Public Health?
READ MORE >

Industry News,
Practice Management
What’s happening with Title X Family Planning?
READ MORE >

Public Health,
Patient Experience
Medical Record Errors: They’re more likely than you think.
READ MORE >

Public Health,
Healthcare Technology
The power of data in a blackout: LHD preparedness & emergency response
READ MORE >
Healthcare Technology
When it comes to EHR adoption, where does public health rank?
READ MORE >

Patient Experience,
Industry News
Patients like the convenience of mobile health but doctors are hesitant. Why?
READ MORE >

Public Health,
Industry News
Are fist-bumps the new handshake for public health?
READ MORE >
Industry News
The Center for Healthy North Carolina releases its latest “Snapshot of Success”
READ MORE >
Load More
Subscribe for More Helpful Content From the Patagonia Health Team!
Need guidance?
Schedule a free 20-minute consultation.
Have questions about how Patagonia Health can meet your needs? Our team of experts is ready to help.